What is sleep paralysis?
Sleep paralysis, that is a sleep disorder that we know and recognize but which still remains quite mysterious, even for scientists. While it can be a symptom of narcolepsy, sleep paralysis can also be isolated and recurrent, meaning it can affect anyone, even people suffering from no other sleep disorder. Perhaps this is where the mystery of this parasomnia lies: everyone can face it! But then, what do we really know about sleep paralysis? Why can this sleep disorder turn into a nightmare? Here are some answers!
How can sleep paralysis be defined?
It is a sleep disorder characterized by an inability to move. One is aware of their state, but the muscle inhibition is such that it is impossible to make movements. Sleep paralysis is a symptom of narcolepsy which is classified as a parasomnia, that is, a sleep disorder characterized by a set of abnormal and undesirable behavioral or psychic events that occur during sleep, or at the boundary between sleep and wakefulness. Recurrent sleep paralysis is a parasomnia of REM sleep, it can be hypnagogic (at the moment of falling asleep) or hypnopompic (at the moment of waking): it is an anomaly of the transition between wakefulness and sleep, or between sleep and wakefulness.
This wake-up paralysis (hypnopompic) can be accompanied by auditory and/or visual hallucinations, making it even more distressing, even traumatic. The association between hallucinations and muscle hypotonia (loss of tone) in a conscious state sometimes results in putting the individual who suffers from it in such a state of fear and helplessness that sleep paralysis leads to mystical interpretations, far beyond science! Besides demons and other evil spirits, this sometimes terrifying phenomenon was described by the writer Guy de Maupassant in his famous fantastic tale “Le Horla”, who must have undoubtedly suffered from episodes of sleep paralysis: “I clearly feel that I am lying down and that I am sleeping... I feel it and I see it... and I also feel that someone is approaching me, watching me, touching me, climbing onto my bed, kneeling on my chest, taking my neck between their hands and squeezing... squeezing... with all their strength to strangle me. I struggle, bound by this atrocious helplessness, which paralyzes us in dreams; I want to scream, I cannot.” Here is a perfect description of this traumatic mystery!
Some figures concerning sleep paralysis
Despite the limited data available to quantify the prevalence of sleep paralysis, Dr. Brian A. Sharpless and his colleagues from the Universities of Pennsylvania and Penn State in the United States crossed data from more than 30 studies involving 35,000 individuals to establish the frequency of this disorder. This analysis from 20111 thus reveals that nearly 8% of the population has experienced or will experience an episode of sleep paralysis “at least once in their life.” This figure rises to nearly 35% for people suffering from diagnosed psychiatric disorders (post-traumatic stress, panic attacks...).
Another epidemiological study from 19992, conducted on a sample of 8,085 European subjects aged 15 to 99 years, highlights the following data concerning the prevalence of sleep paralysis:
- 6.2% of participants experienced at least one episode of sleep paralysis during their lifetime
- 1.4% of participants experienced moderate sleep paralysis (at least one episode per month)
- 0.8% of participants experienced severe sleep paralysis (at least one episode per week)
What are the causes of sleep paralysis?
To date, scientifically speaking, it is still difficult to establish the exact causes of sleep paralysis. However, cross-referencing various studies tends to highlight common factors among victims of this sleep disorder. One study3 clearly demonstrates that poor sleep quality is a cause regularly associated with sleep paralysis. Furthermore, other factors4 have been highlighted to explain it:
- fatigue, poor sleep quality, insomnia
- anxiety
- post-traumatic stress, depression
- sudden lifestyle change (new job, bereavement, change of living environment…)
- suffering from narcolepsy
It is therefore observed that people suffering from sleep disorders (insomnia, narcolepsy) are not more exposed than others, even if individuals with diagnosed behavioral disorders seem more prone to be victims of episodes of sleep paralysis.
How does sleep paralysis manifest?
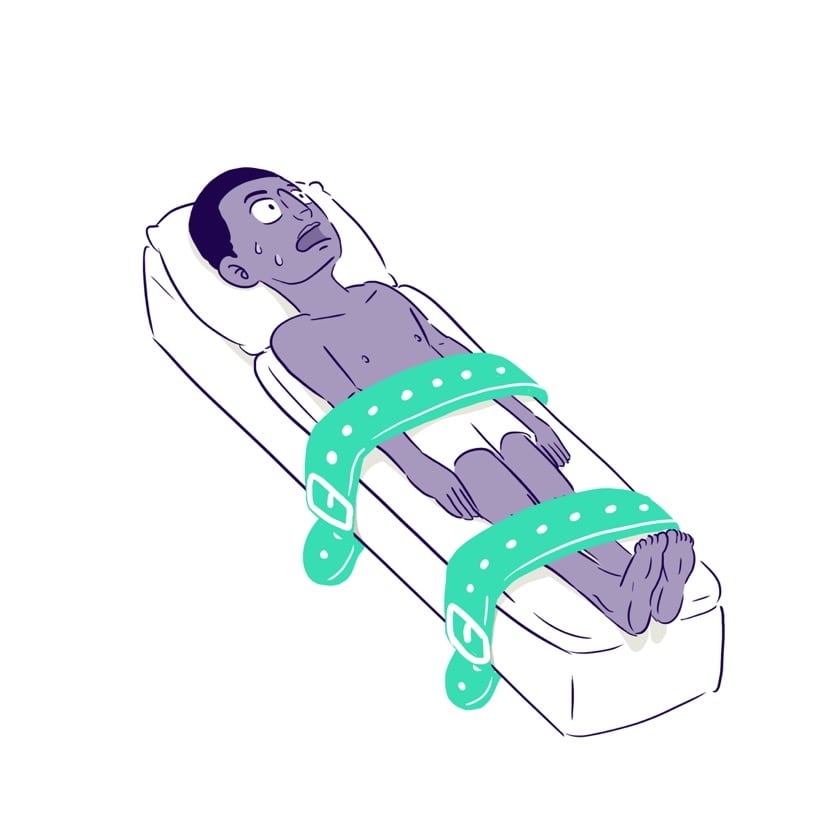
When we are in the phase of REM sleep, our body is in a state of paralysis called “muscle atonia.” This muscle atonia is caused by the brain to prevent the body from injuring itself during sleep. It is programmed to stop by itself at the moment of waking. However, the episode of sleep paralysis comes from the fact that awakening occurs during a phase of REM sleep, a time when brain activity is intense but without communication between the muscles and the brain. We thus find ourselves in a waking state but unable to act on our muscles because the brain is still in “muscle atonia” mode.
While sleep paralysis is not dangerous, in itself, for health or the body, it can nevertheless be very traumatic in its most extreme form, when accompanied by particularly distressing hallucinations. The experience of body paralysis then turns into a wakeful nightmare. The psychological aftereffects of this trauma can be more or less significant depending on the individual. Some testimonies from people who have been victims of episodes of sleep paralysis5 are very telling and leave no one indifferent, even inspiring movie scenarios! A striking documentary, “The Nightmare6,” was made by Rodney Ascher, himself a victim of episodes of sleep paralysis. Far from exaggerating the terrifying aspect of this parasomnia, it offers perhaps a more realistic and objective view through various testimonies.
In fact, sleep paralysis can be described as “wake-up paralysis” when it is hypnopompic.
Here are the main symptoms of sleep paralysis, recorded by various studies7:
- inability to move
- feeling of wakefulness
- sensation of suffocation, feeling of weight on the chest
- auditory hallucinations, visual hallucinations

How can sleep paralysis be diagnosed?
The diagnosis of sleep paralysis is based on clinical signs collected from individuals during the different episodes they experience. A consultation with a doctor is then necessary to evaluate medical history as well as to identify the different disorders that may be associated with sleep paralysis: behavioral disorders, emotional shock, sleep disorders, or anxiety. Sleep disorders such as insomnia or narcolepsy must be taken into account. Monitoring sleep phases by means of a polysomnography allows recording electrical activity in the muscles, thus characterizing sleep paralysis by noting a low level of this electrical activity.
Thus, according to some studies8, sleep quality and associated disorders (insomnia, narcolepsy, fatigue, nightmares), as well as some behavioral disorders, could help diagnose sleep paralysis.
How can sleep paralysis be treated?
There is no specific treatment to cure sleep paralysis. However, one can try to treat some of the supposed causes of this phenomenon9, namely:
- improve sleep quality by going to bed at a fixed time and avoiding sleep deprivation as much as possible
- combat sources of stress and anxiety (for example through relaxation techniques)
- prescription of antidepressants to limit episodes of sleep paralysis, especially when associated with narcolepsy
Sleep paralysis is not dangerous for the physical integrity of those who suffer from it. Nevertheless, it remains stressful and distressing for the majority of people who suffer from it due to the association between the conscious state in which one finds oneself and the paralysis it causes, not to mention possible hallucinations. While it can affect anyone when we talk about isolated recurrent paralysis, its form associated with narcolepsy is more severe.
To complement the discussion on sleep paralysis, here is a link to a “Ted” video (“The Terrors of Sleep Paralysis” by Ami Angelowicz) which very well illustrates this surprising and mysterious phenomenon!
Sources :
[1] Lifetime prevalence rates of sleep paralysis: A systematic review, Brian A. Sharpless, Jacques P. Barber, “Sleep Medicine Reviews”, October 2011 [2] Prevalence and pathologic associations of sleep paralysis in the general population , M.M. Ohayon, J. Zulley et al, “Neurology”, April 1999 [3] Relationships between sleep paralysis and sleep quality: current insights, Dan Denis, “Nature and Science of Sleep”, November 2018 [4] What You Should Know About Sleep Paralysis, site « SleepFundation », 2020 [5] The frightening experience of sleep paralysis, the wakeful nightmare, site « rtbf.be », 2018 [6] The Nightmare, official trailer, excerpt from the documentary, site « Youtube », 2015 [7] Isolated sleep paralysis, N.S. Sawant, S.R. Parkar et al, “Indian Journal of Psychiatry”, October-December 2005 [8] Relationships between sleep paralysis and sleep quality: current insights, Dan Denis, “Nature and Science of Sleep”, November 2018 [9] Sleep disorders in children and adults, site « Collège des Enseignants de Neurologie », 2020
